5 Ways To Prevent Antibiotic-Resistant Salmonella Typhi
By Laurel Maloy, contributing writer, Food Online
Prevention is often facilitated with the most basic sanitation procedures and applied safety measures
The former Undersecretary of Agriculture for Food Safety Dr. Richard Raymond blogged recently about his upcoming travel plans for Meatingplace. This would not have been an “event” so-to-speak, except for the fact the blog’s title starts with Salmonella Typhi. That’s an attention-getter, especially when he talks about voluntarily infecting himself with five BILLION Salmonella Typhi colony-forming units. What?
According to his blog account, after he gets done with the “Ebola cities tour” (his words) of Dallas, Atlanta, and Omaha — he will be flying to Jakarta, Indonesia, to meet with cattle producers there. Jakarta, it turns out, does not have much of a public health system. As a result, travelers face the very real threat of contracting Salmonella Typhi, more commonly known as typhoid fever. In an effort to prevent this from happening, the Centers for Disease Control and Prevention (CDC) and the State Department will be helping the good doctor to vaccinate himself, thus reducing his possibility for infection while traveling. Raymond will be taking a prophylactic treatment of four capsules, one every other day. An injectable vaccine is also available, either of which must be completed at least one to two weeks prior to possible exposure. His tongue-in-cheek blog finds irony in the fact that he’s spent years of his life talking about water and foodborne-illnesses, only to be purposefully choosing self-contamination.
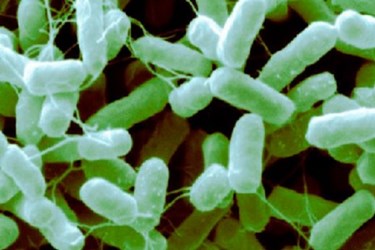
Salmonella Typhi, also a threat here in the U.S., is most common in developing countries, where approximately 21.5 million persons contract the disease each year. In the U.S., the CDC estimates about 5,700 cases annually, with the majority, about 75 percent of the cases, the result of traveling internationally. According to the CDC, Asia, Africa, and Latin America are the most dangerous for U.S. travelers, as evidenced over the last 10 years. That still leaves about 1,500 non-traveling U.S. citizens faced with this particular life-threatening illness annually due to local food- or water-borne contamination. It is passed from person to person by ingesting food or water infected with the pathogen. Those with typhoid fever, in addition to those who just carry the disease and are asymptomatic, will shed the pathogenic cells in their stools (feces). The most common source of contamination is from sewage-infected water or from foods washed or irrigated with contaminated water. Neglecting the most basic sanitation procedures, such as frequent hand washing, can easily cause the spread of this germ to the unsuspecting.
Based on the facts known about Salmonella Typhi, prevention is the key. Salmonella Typhi is closely related to both Salmonella Typhimurium and Enteritidis, as are between 95 and 99 percent of all Salmonella bacteria. The latter two strains above are the most common forms of food poisoning, with Salmonella Typhimurium being replaced in recent history with the Enteritidis bacterium. Salmonella Typhi, unlike these other two strains, is considered exceptionally dangerous and often fatal. Infection is further complicated by the fact that the Salmonella that causes typhoid fever is becoming increasingly resistant to the antibiotics routinely used to treat it. Antibiotic use in food animals has long been under fire by consumers and advocacy groups. More recently, the American Medical Association (AMA) and a Consumer Reports poll provide insight to how the healthcare community views the threat. Eighteen pathogens, including four foodborne enteric pathogens — Campylobacter, Nontyphoidal Salmonella, Salmonella Typhi, and Shigella — were all central to a CDC report released called Antibiotic Resistance Threats in the United States, 2013.
Here are ways to prevent Salmonella Typhi in your facility:
- Ensure agricultural and industrial water is pathogen free. The Food Safety Modernization Act (FSMA) addresses this issue, and is currently in the process of revising its irrigation water standards.
- Encourage and monitor employee hand washing and the routine use and frequent changing of sterile gloves.
- Monitor employee health, especially if an employee has traveled to a developing country where typhoid fever is prevalent. Symptoms of typhoid fever include a fever of 103°F to 104°F, sometimes accompanied by a rash. Patients may also exhibit weakness, headaches, stomach pains, or a loss of appetite. Stool or blood sampling is the only way to rule out typhoid fever.
- Employees regularly traveling to developing countries should be vaccinated against typhoid fever. The vaccine can lose its effectiveness after several years, so keep good records and encourage revaccination. The oral vaccine is good for five years, while the injectable vaccine requires a booster every two years.
- Pay particular attention to raw fruits and vegetables that cannot be peeled or easily washed, such as lettuce, broccoli, cauliflower, and artichokes. Include in your sanitation standard operation procedures (SSOP) or your hazard analysis and critical control points (HACCP), the means by which to prevent and to monitor the results of your facility’s washing protocols.
While specifically addressing the prevention of Salmonella Typhi, these same sanitation procedures are an adequate means by which to prevent many foodborne pathogens from reaching consumer tables.
